
To clarify, a sponsor is a party that pays for the benefits plan, and the payer (insurance company) administers the insurance product.

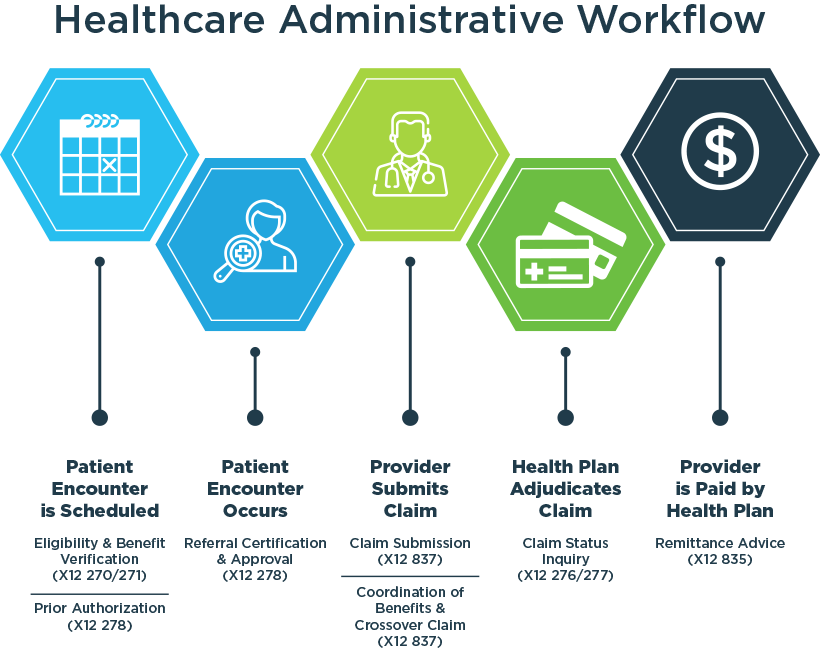
The Health Insurance Portability and Accountability Act (HIPAA) requires that specific administrative processes must use standardized electronic transactions.ĮDI 834 establishes a seamless communication between the sponsor of an insurance product and the payer. This transaction set is used by employers, government agencies, enrolling members, insurance agencies, union agencies, and others included in a healthcare benefits plan. Defining EDI Benefit Enrollment and MaintenanceĮDI 834 is a transaction set representing the Benefits Enrollment and Maintenance document. Using 834 EDI files instead of paper checks and explanations of benefits helps reduce administrative costs for both insurance companies and healthcare providers. The EDI 834 files simplify and automate the payment recording process for providers. Providers use the EDI 834 files to ensure accurate recording of payments in their accounting systems. It includes details like patient information, claim number, total payment amount, adjustment amounts, and remittance information for each claim. The EDI 834 transaction set contains information about claim payments from insurance companies to providers. What is EDI 834 file and transaction set?Īn EDI 834 file is used to electronically transmit health care insurance claim payment data between insurance companies and health care providers. Today, 834 files are used for the vast majority of health insurance claim payments, creating efficiencies and cost savings for both insurers and providers compared to the old paper-based payment processes. Since then, the use of 834 files has grown significantly as major health insurers and providers implemented EDI systems. The EDI 834 standard was adopted formally in 1998 by the Health Care Administrative Simplification Compliance Act and later included in HIPAA legislation. The goal was to reduce costs and errors by automating an important but time-consuming administrative process. The 834 EDI transaction set was created to electronically transmit health insurance claim payment information. Paper-based healthcare transactions were slowing down the system, so industry groups worked with the federal government to establish EDI transaction standards. Whether you are a healthcare professional, a benefits administrator, or simply curious about the subject, this guide will provide valuable insights and information on 834 EDI transactions.ĮDI 834 files were developed in the 1990s as part of a broader push to transform healthcare administrative processes using electronic data interchange (EDI). In this article, we will delve into the history of EDI 834 transactions and the standard way to exchange enrollment data via ASC and HIPAA 834– Benefit Enrollment and Maintenance File format. From insurance agencies and government bodies to unions and employers, EDI 834 transactions are widely used in the employee benefits administration process. This information includes details about the payer, sponsor, and members involved in offering benefits products. Understanding how EDI 834 transactions work can help businesses streamline their operations and improve communication with their partners and clients.ĮDI 834 transactions play a crucial role in facilitating the transfer of enrollment and maintenance information. Electronic Data Interchange (EDI) is a crucial component for exchanging data for the healthcare industry as it heavily relies on EDI. But that’s not it! There is a lot of work that goes behind the curtains, such as enrollment files, member maintenance files, plan data, billing data, and rating data.
Edi testing 834 filr testing forum full#
When thinking of a private health insurance exchange, you just think of a marketplace full of options.


 0 kommentar(er)
0 kommentar(er)
